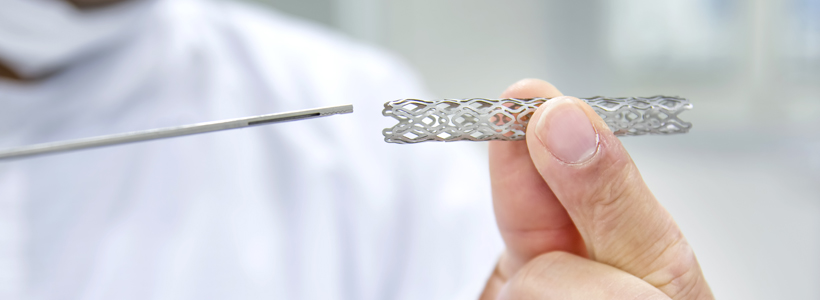
Percutaneous coronary intervention (stent)
The main focus of Dr Hendricke’s practice is the field of percutaneous coronary intervention. This field of cardiology involves catheter-based, minimally invasive intervention. The route of access to the heart is preferably via the radial artery route in > 95% of cases, but for various reasons, the femoral artery is used.
Interventions involve the insertion of a coronary guidewire beyond the point of obstruction and the insertion of an inflatable balloon and usually a drug-eluting stent to scaffold the diseased artery. Excellent stent expansion is mandatory in order to prevent abrupt vessel closure, due to stent thrombosis, a possibly fatal complication.
Various techniques to visualise the stent are employed, the most recent innovation being optical coherence tomography, a near-infrared spectrum light probe technique used to assess vessel characteristics and stent deployment to augment therapeutic and diagnostic decisions. Intravascular ultrasound is also used for the same purposes, but with subtle differences.
In the event of severe, calcified (hard) plaque being present, Rotablation is used. This technique involves using an ultra-high-speed rotational atherectomy device to debulk the plaque (rotational speeds of > 160 000 rpm usually). This is a highly specialised technique, and well tolerated usually.
The main direction of Dr Hendrickse’s Practice is coronary intervention guided by international standards, best local practices and modern literature.

